Anger is a sudden maladaptive response to a variety of stimuli characterised by an aggression which could be verbal, physical or both. It is provoked more often in people with a certain personality types especially when subjected to stressful triggers or situations in specific contexts. It may even be provoked by minor stimuli in anyone depending on the circumstance. While it has been essential for the survival of our species, modern life (in overcrowded urban jungles) provides too many stressors that provoke unnecessary anger which then has long term health implications. This article attempts to throw some light as to the causes, effects and changes during and after an episode of Anger.
Civilisation and urbanisation forces people of all different personality types, of different interests and priorities to live together. In the hustle and bustle of daily living we are forced to deal with different situations and people who could make our lives difficult, with intention or otherwise. We are provoked into losing our tempers, get angry, explode (or implode) and suffer the consequences. Our personality type, our current mental state, our previous experiences, the people we have to deal with, all have a role in determining how we respond to a situation and how angry we get. Often we get irritated with what is happening and if this isn’t resolved, results in anger. I call Anger a maladaptive response because we get angry only with people we can get away with showing it and it rarely solves the issue that provoked it.

The Anger reaction begins in the Amygdala in the brain, it spread to the Hypothalamus and the Pituitary which releases ACTH hormone that stimulates Cortisol secretion from the Adrenal glands. Cortisol suppresses the immune system, increase sugar production and the conversion of Fatty acids to energy. The adrenals also produce Adrenaline which increase the Heart rate BP and the Cardiac output. Adrenaline also increases the release fo glucose from the Liver and increases the tension in the skeletal muscle and also increasing the rate and force of contraction of the skeletal muscles. The respiratory rate increases and visual fields constrict and pupils dilate allowing the angry person to focus on the person triggering the reaction. In short the body prepares for “fight or flight” when angry.
All these hormones increase the blood pressure, Heart rate and respiratory rates. Blood is shunted away from “nonessential” organs such as the intestine and kidneys in favour of the heart lung brain and skeletal muscles. It is quite common to feel like you want to empty your bladder or even vomit when very stressed.

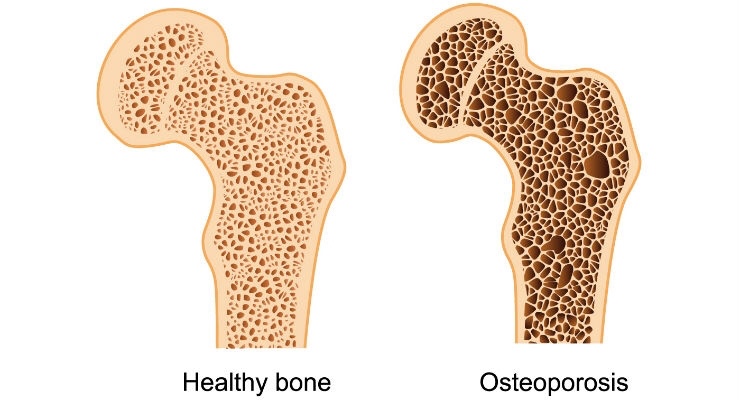
Chronic and recurrent Anger depletes the body’s ability to fight inflammation that is triggered by the free radicals. This eventually causes disease.
Anger is known to cause frequent headaches, digestive problems and abdominal pain/gastritis, Insomnia, increased anxiety and depression, skin problems and eczema and even Heart attacks and Strokes.
Your Anger has not only implications for you, your mental and physical well being and productivity but also for that of your family, friends, work colleagues and everyone in your immediate surroundings. Your anger will have a domino effect on others. It is therefore very important to control or release your anger, not just for your own selfish reasons but also for the greater good of society.
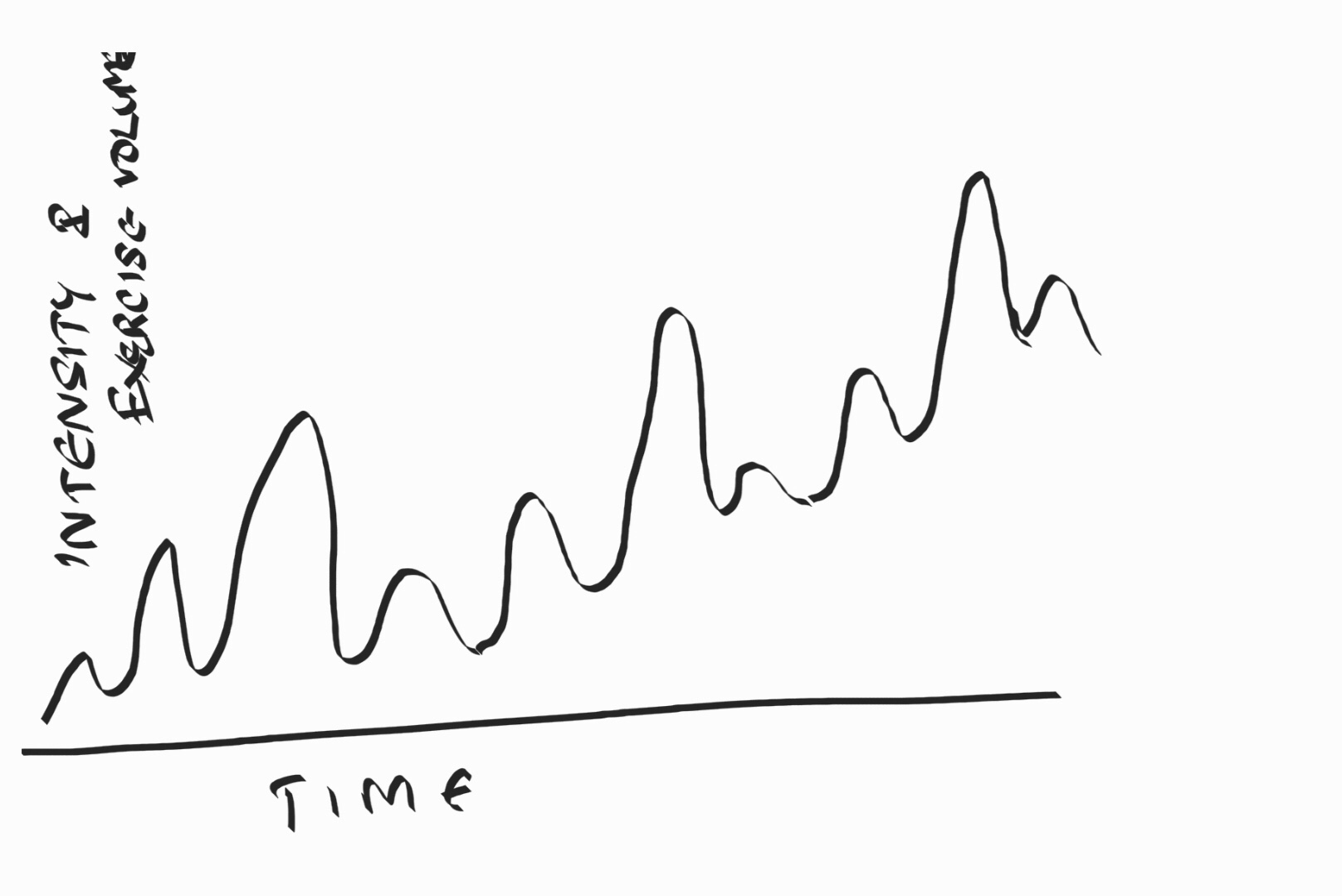
The first step in Anger management would be to realise that Anger is harmful to you more than to anyone else. While there may be many ways to keep your anger in control, I personally believe that if you have an understanding nature, have empathy for others and make excuses (to yourself) for their inability to see or do things your way – you could control your anger. Being placid or timid or avoiding people or situations may not necessarily be the right way to deal with anger or a situation that could make you angry. Learning to meditate, attempting to resolve conflict by understanding the other person and seeking counselling (professional) could help you deal with your anger. Yoga, exercise, regular breaks from your work, having a supportive network of friends and family could also help you release your anger. Keeping a diary could help you understand your anger and could help you device strategies to cope with stressful situations when they happen the next time.
My very best wishes to you for staying cool always.

You must be logged in to post a comment.